|
| Image Credit: Gregory Wanner, DO PA-C |
 |
| This post was peer reviewed. Click to learn more. |
Author: Gregory Wanner, DO PA-C
Emergency Medicine Resident, PGY-3
AAEM/RSA Publications Committee Chair ’16-’17
Author: Dimitrios Papanagnou, MD, MPH, EdD(c)
Assistant Professor, Emergency Medicine
A version of this article was previously published on the Jefferson Emergency Medicine Residency Blog (www.jeffem.org), March 2016.
It’s 3 am on a Saturday and you’re covering the emergency department at a community hospital. You hear a nurse’s firm but slightly nervous-sounding voice from down the hall say, “Umm, I need some help in here.”
You enter the room and find a geyser of blood erupting from the mouth of a middle-aged, male patient. His family informs you that he is a heavy drinker and has “liver problems”.
What do you do?
After applying triple-G protection (gown, gloves, and goggles), you slide towards the patient and begin to perform the critical actions associated with establishing large bore IV access, securing the airway, transfusing blood, starting octreotide, and calling GI. The patient keeps bleeding. He is severely hypotensive and GI is unavailable.
What else can you do?
The patient is exsanguinating likely from an esophageal variceal bleed. You have tried all other options and GI is not able to help. At this point, the use of a gastroesophageal balloon tamponade tube (GEBT) should be considered. The GEBT — more commonly known as a Sengstaken-Blakemore tube or Minnesota tube — is infrequently used and its placement is rarely practiced. However, it may be potentially life saving in certain situations.
What is a GEBT tube?
Two types of GEBT tubes are most often available: The 3-lumen Sengstaken-Blakemore tube (often just referred to as a “Blakemore”) or the 4-lumen Minnesota tube. The Blakemore includes a gastric balloon, esophageal balloon, and a gastric aspiration port. The Minnesota tube adds an esophageal aspiration port as well. The function of both tubes is similar — to apply internal pressure in an attempt to stop gastric or esophageal variceal bleeding.
When would I consider using a GEBT tube?
This device is considered as an option of last resort. A “Hail Mary” play when other treatments have failed and the patient has a high risk of mortality. Starting medications (octreotide), volume replacement (blood products), and a discussion with GI should, ideally, occur before using a GEBT tube. Major complications from the GEBT tube, such as esophageal perforation, occur in up to 16% of patients. Mortality directly related to GEBT tube use is 3-6%. Variceal hemorrhage mortality, however, ranges from 20-80% depending on the reference. [1-2]
How do I use a GEBT tube?
Attempting to learn how to use a GEBT tube while a patient is actively hemorrhaging in front of you is not ideal. A better method would be to review some teaching materials beforehand. Here are some resources:
- Printable bedside step-by-step instructions with photos (PDF) [3]
- Run a GEBT simulation case: Our MedEdPortal sim case with teaching files (free download with free login) [3]
- EMCrit video and instructions [4]
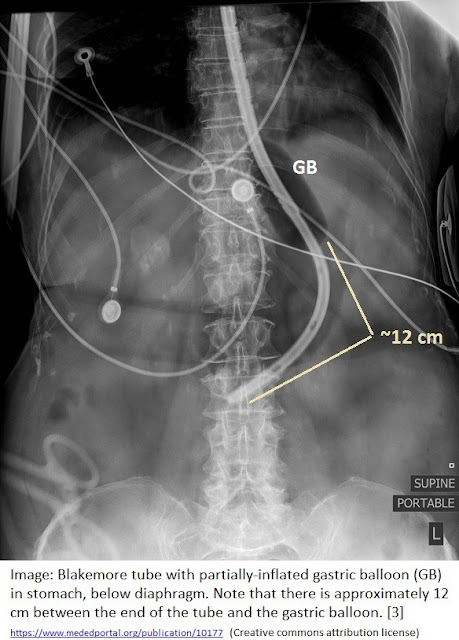
- Radiographic image showing GEBT placement [3]
Make your own GEBT kit!
To avoid running around the ED when a critical variceal bleeder comes in, consider putting all of these items together in a kit.
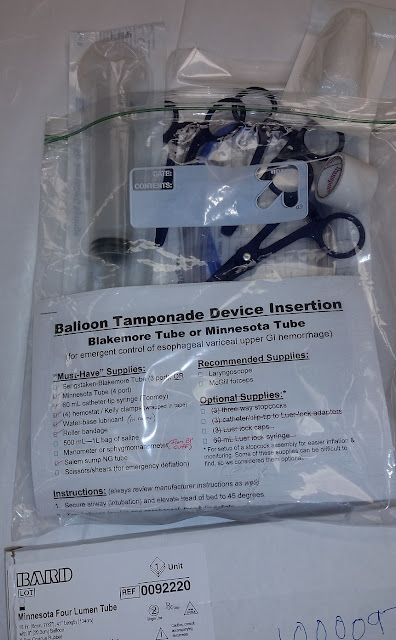 |
| Image Credit: Jefferson EM Residency Blog |
Learn the steps and review this information NOW—before the exsanguinating patient comes in.
References:
1. Cook D, Laine L. Indications, technique, and complications of balloon tamponade for variceal gastrointestinal bleeding. J Intensive Care Med. 1992; 7(4): 212-218. PMID: 10147943
2. Winters ME, Panacek EA. Balloon Tamponade of Gastroesophageal Varices. In: Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine. 6th ed. Philadelphia, PA: Saunders Elsevier; 2014: 831-836.
3. Wanner G, Papanagnou D. Massive Upper Gastrointestinal Bleeding with Gastroesophageal Balloon Tamponade. MedEdPORTAL Publications; 2015. Available from: https://www.mededportal.org/publication/10177
4. Weingart S. Blakemore Tube Placement for Massive Upper GI Hemorrhage. EMCrit website. http://emcrit.org/procedures/blakemore-tube-placement October 13, 2013. Accessed March 5, 2016.