 |
| Image Credit: Subhadra Jalal – Flickr |
Author: Stephanie Cihlar, MSIII
Medical Student
Loyola University Chicago Stritch School of Medicine
AAEM/RSA Publications Committee Member
 |
| This post was peer reviewed. Click to learn more. |
Introduction
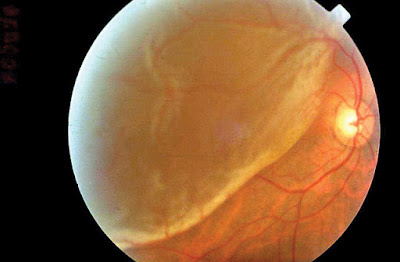
Retinal detachment is one of the most common ophthalmic emergencies, affecting approximately 1 in 10,000 people per year.[1] Because of the risk of permanent vision loss, it is important that emergency physicians are able to identify a retinal detachment and consult a retinal specialist as soon as possible.
Pathophysiology
Retinal photoreceptors (rod and cones) are metabolically highly active cells. In fact, the choroidal circulation responsible for nourishing these cells has the highest blood flow per cubic centimeter of tissue found in the human body.[2] In a retinal detachment, the neurosensory layer of the retina is peeled away from its underlying supporting tissues, the retinal pigment epithelium and choroid. The photoreceptors undergo ischemic damage, which can lead to vision loss and blindness in a matter of hours.[3]
Most retinal detachments occur when a portion of the retina is torn and fluid leaks between the retinal layers. The most common cause of a retinal tear is a posterior vitreous detachment (PVD). PVDs occur when the gelatinous vitreous humor liquefies and pulls away from the retina. During this process the vitreous can pull a portion of the retina with it and cause a tear.[4]
Other important causes of retinal detachment are trauma, neovascularization retinopathies, and degenerative conditions that cause an abnormal thinning of the retina.[4][5]
Signs/Symptoms
Patients suffering from a retinal detachment will classically present with:
- Flashes- Also called photopsias, flashes are short bursts of light in the peripheral vision. These are due to traction of the vitreous humor pulling on the retina.
- Floaters- Clear to black specks or strings in vision caused by clumps of tissue or blood in the vitreous.
- Visual field loss – Often described as a curtain, veil, or shadow being pulled down or across the visual field. The visual field loss is often preceded by flashes and floaters for days to weeks.
- Aging
- Myopia (the greater the refractive error the greater the risk)
- Posterior vitreous detachment
- Previous ocular surgery
- Ocular trauma
- Family history of retinal detachment
- Diabetic retinopathy
- Sickle cell retinopathy
- Retinopathy of prematurity
- Certain genetic disorders such as Marfan’s syndrome and Stickler’s syndrome
- Preexisting retinal disorders such as lattice degeneration of the retina
- Presence of acute retinal infections (as in acute retinal necrosis syndrome or CMV retinitis)
Differential Diagnosis and Evaluation[8]
A careful history helps distinguish retinal detachment from other conditions with similar symptoms.
- Floaters that occur with retinal detachment are often more abrupt and dramatic than benign floaters that occur with aging.[6]
- Flashes in a retinal detachment are unilateral which distinguishes them from migraines and most strokes.[6]
- The location of the visual field loss, or scotoma, is another important clue. In retinal detachment, visual field loss typically starts in the periphery and progresses to involve central vision over hours to weeks.[6] Conversely, if the scotoma involves only the central vision, it could indicate a problem with the macula such as macular degeneration, a retinal artery or vein occlusion, or an optic neuropathy. [6]
- If the vision loss is episodic instead of constant and progressive, consider transient ischemic attack or ocular migraine.[6]
It is also important to ask about any preexisting eye conditions, history of eye surgeries or trauma, and family history of retinal detachment.
In addition to taking a detailed history when retinal detachment is suspected, it is important to evaluate visual acuity, visual fields, extraocular motility, and check for a relative afferent pupillary defect. Patients with a suspected retinal detachment and decreased visual acuity or monocular decreased visual fields should be seen emergently by an ophthalmologist, definitely within 24 hours.
Diagnosis
A definitive diagnosis is made by an ophthalmologist on dilated eye examination. If the retina cannot be visualized on dilated eye exam (for example due to a dense cataract or bleeding in the vitreous), or if an ophthalmologist is not available for consult, ocular ultrasonography may be used by trained ED clinicians for diagnosis.[9]
Next Steps
After diagnosis of retinal detachment, the consulting ophthalmologist will typically decide how soon the patient needs to be seen by a retinal specialist. It is ideal for patients to be seen within 24 hours to minimize permanent vision loss.[10] The retinal specialist will decide which procedure is most appropriate based on the location and type, and severity of the detachment.
The most common treatments are:
- Laser photocoagulation- For retinal tears, before significant detachment develops. Creates a chorioretinal scar that prevents fluid from entering the subretinal space.[6,11]
- Pneumatic retinopexy- A bubble of gas is injected into the vitreous space. The patient lays face down to allow the bubble to push the retina back into place.
- Scleral buckle- in the operating room, a band is placed around the sclera in order to form an indentation, which seals the retinal tear.
- Vitrectomy- Intraoperatively, the retina is flattened using a long-acting air bubble or heavier liquid.[6]
References
1. Wilkes SR, Beard CM, Kurland LT, Roberson DM, O’Fallon WM. The incidence of retinal detachment in Rochester, Minnesota, 1970-1978. Am J Ophthalmol. 94(5):670. http://www.ncbi.nlm.nih.gov/pubmed/7148948
2. Bill A. Circulation in the eye. Handbook in physiology. 1984; 1001-34.
3. Ghazi N, Green W. Pathology and pathogenesis of retinal detachment. Eye. 2002;16(4):411. http://www.ncbi.nlm.nih.gov/pubmed/12101448
4. Hikichi T, Trempe CL, Schepens CL. Posterior vitreous detachment as a risk factor for retinal detachment. Ophthalmology.1995; 102(4):527. http://www.ncbi.nlm.nih.gov/pubmed/7724167
5. Podgor MJ, Leske MC, Ederer F. Incidence estimates for lens changes, macular changes, open-angle glaucoma and diabetic retinopathy. Am J Epidemiol. 1983; 118:206-12. http://www.ncbi.nlm.nih.gov/pubmed/6881126
6. Gariano RF, Kim CH. Evaluation and management of suspected retinal detachment. Am Fam Physician. 2004; 69(7):1691-8. http://www.ncbi.nlm.nih.gov/pubmed/15086041.
7. Jalali S. Retinal Detachment. Community Eye Health. 2003;16(46):25-26. http://www.ncbi.nlm.nih.gov/pubmed/17491854
8. Brown GC, Brown MM, Fischer DH. Photopsias: a key to diagnosis. Ophthalmology. 2015;15(2)613. http://www.ncbi.nlm.nih.gov/pubmed/26249730
9. Vrablik, Michael et al. The Diagnostic Accuracy of Bedside Ocular Ultrasonography for the Diagnosis of Retinal Detachment: A Systematic Review and Meta-Analysis, Annals of Emergency Medicine. 2015; 66(3):342-343. http://www.ncbi.nlm.nih.gov/pubmed/26304260
10. Prabhat P, Sanaz A. Ocular Emergencies. Am Fam Physician. 2007; 76(6): 829-836. http://www.ncbi.nlm.nih.gov/pubmed/17910297
11. Gerstenblith AT, Rabinowitz MP. The Wills Eye Manual, Office and Emergency Room Diagnosis and Treatment of Eye Disease. Philadelphia: Lippincott Williams & Wilkins; 2012.
