|
| This post was peer reviewed. Click to learn more. |
Emergency Medicine Resident
Adena Regional Medical Center
Ischemic heart disease and coronary artery disease (CAD) are two of the leading causes of death among adults in developed countries.[6] Patients with these disorders can present to the emergency department with problems that fall anywhere along the spectrum of clinical diseases referred to as acute coronary syndrome (ACS). ACS is the result of myocardial ischemia and can range from unstable angina to ST-segment elevation myocardial infarction (STEMI) that requires emergent intervention. STEMI requires immediate recognition; however not all STEMIs present with elevations on the initial standard 12-lead electrocardiogram (ECG).[1]
In general, ECGs provide a rapid way to evaluate for signs of cardiac ischemia and rhythm disturbances. While the ECG is one of the best tests in the emergency department to assess and evaluate the evolution of ACS, ECGs have limitations. One of these limitations is the inability to evaluate the posterior wall.[3,6]
Posterior myocardial infarctions contribute to 15-20% of all acute myocardial infarctions (AMIs) and occur in isolation in about 4% of AMIs.[2] The lesions contributing to posterior infarctions may be found in the right coronary artery, its posterior descending branch, or the left circumflex artery.[5] They are often hard to recognize and diagnose because they lack the ST-elevations seen in a “classic” STEMI.[1,3] They often present with ST segment depression in ECG leads V1-V3.[1,2,3]
ST segment depression is generally considered subendothelial or non-infarction ischemia and is associated with non-ST-segment elevation myocardial infarctions (NSTEMI). However, these depressions may precede ST-segment elevation in a STEMI or they may be reciprocal ST-segment changes from the “opposite” side of the heart. When they are seen in V1-V3, depressions can represent a “mirror image” of ST-segment elevation from a posterior STEMI.[6]
Diagnosis of posterior STEMI requires differentiating reciprocal changes from depressions due to NSTEMI.[1] Evidence of ST segment depression in V1-V3 needs to be further evaluated by looking at the posterior leads of the ECG.[1,2,3,5]
The easiest way to obtain these leads is to move leads V5 and V6 to V8 and V9. These lead positions are found at the inferior angle of the scapula (V8) and the left paraspinal area (V9).[7] Alternatively, a formal posterior ECG can be performed by placing the precordial leads on the back as a “mirror” image of the front.[6]
Criteria for diagnosis of posterior STEMI include:[1]
- ST-depression ≥0.5mm in leads V1-V3.
- Associated T-waves are either upright or inverted.
- Appearance of tall R-waves in V1-V2 (may be delayed).
- Recommended: posterior chest wall leads (V7-V9 ≥0.5 mm* ST-elevation).[1]
*may be decreased secondary to increased distance of posterior leads from heart.[6,7]
Due to the complexity of diagnosing a posterior myocardial infarction, door-to-balloon times are significantly longer for isolated posterior infarctions than non-posterior myocardial infarctions.[4] Some of this delay is secondary to the time it takes to get an ECG with posterior leads. To reduce the evaluation time, some clinicians will perform the “flip test.” This involves turning the initial ECG paper over to look at the back of the upside-down paper. Holding the paper up to a light will enable visualization of ST-elevation and Q waves in leads V1-V3 that correlates with posterior STEMI. This provides more information but is not as accurate as direct visualization of the posterior leads.[8]
The ECG showing signs of ST-segment elevations elicits a “STEMI Alert” and allows the patient to have their myocardium reperfused as quickly as possible. When the ST-segment is elevated, time is cardiac muscle. However, not all ST-segment elevations are as easy to spot as others.
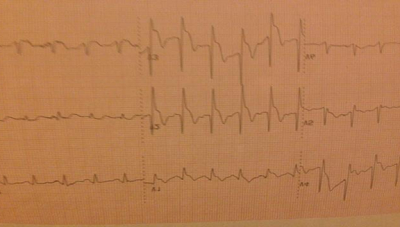
Below are ECGs from an example case (from Adena Regional Medical Center):
Cardiac catheterization showed 100% stenosis of the ramus (a third branch of the left coronary artery arising between the left anterior descending and circumflex coronary arteries), 90% stenosis of the mid circumflex, and 90% stenosis of the right coronary artery.
References:
1. Rokos IC, French WJ, Mattu A, et al. Appropriate cardiac cath lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J. 2010;160(6):995-1003, 1003.e1-8.
2. Brady WJ. Acute posterior wall myocardial infarction: electrocardiographic manifestations. Am J Emerg Med. 1998;16(4):409-13.
3. Khan JN, Chauhan A, Mozdiak E, Khan JM, Varma C. Posterior myocardial infarction: are we failing to diagnose this?. Emerg Med J. 2012;29(1):15-8.
4. Waldo SW, Brenner DA, Li S, Alexander K, Ganz P. Reperfusion times and in-hospital outcomes among patients with an isolated posterior myocardial infarction: insights from the National Cardiovascular Data Registry (NCDR). Am Heart J. 2014;167(3):350-4.
5. Brown L, Sims J, Conforto A. Posterior myocardial infarction with isolated ST elevations in V8 and V9: Is this an “ST elevation MI”?. CJEM. 2003;5(2):115-8.
6. Rosen, Peter, John A. Marx, Robert S. Hockberger, Ron M. Walls, and James Adams. “Acute Coronary Syndrome.” Rosen’s emergency medicine: concepts and clinical practice. 6th ed. Philadelphia, Pa.: Mosby Elsevier, 2006. 947-983. Print.
7. Mattu, Amal, and William Brady. “Part One.” ECGs for the emergency physician. London: BMJ. 2003. 63. Print.
8. Rezaie Salim. Posterior Myocardial Infarction: How Accurate is the Flipped ECG Trick?. Academic Life in Emergency Medicine. August 7, 2013. Available athttp://www.aliem.com/posterior-myocardial-infarction-how-accurate-is-the-flipped-ecg-trick/. Accessed 12/24/2014