Authors: Tim Montrief, MD MPH and Mehruba Anwar Parris, MD FAAEM
AAEM/RSA Publications & Social Media Committee and Common Sense Assistant Editor
Originally published: Common Sense May/June 2019
Case
A 25-year-old Caucasian male with no significant known past medical history presented to a community emergency department via EMS with palpitations and altered mental status while on vacation at a friend’s bachelor party. Per the patient’s friend, he had been drinking alcohol all day and accidentally ingested a large amount of smokeless tobacco one hour prior to arrival, with subsequent nausea, vomiting, and excessive salivation. His friend denied any co-ingestions or drug use. The patient was found to be somnolent but arousable to voice, without any focal neurologic deficits and normal point of care blood glucose. The initial physical exam was remarkable for new-onset atrial fibrillation with a heart rate in the 160’s, blood pressure of 102/56 mmHg, respiratory rate of 16 breaths per minute, and saturating 100% on room air. Aside from atrial fibrillation with rapid ventricular response, the electrocardiogram was unremarkable (Figure 1). Additionally, the chest X-ray showed no evidence of cardiopulmonary pathology. Further testing revealed normal troponin, T4, and TSH levels. He had an elevated serum alcohol level of 191 mg/dL, and a negative urine drug screen. Initial cotinine and nicotine levels were not available. The patient was given a diltiazem bolus and drip, as well as four liters of lactated ringers, with subsequent heart rates in the low 100’s, with corresponding blood pressures in the 120’s/80’s. The patient was admitted to the ICU, and spontaneously converted back to a normal sinus rhythm within 24 hours of his initial presentation. The patient was discharged the next day with close outpatient follow-up.
 |
| Figure 1. Initial ECG, showing atrial fibrillation with rapid ventricular response at a rate of 150 beats per minute, and normal PR/QT/QRS intervals. |
What do we know about smokeless tobacco and nicotine toxicity?
Smokeless tobacco products contain either air- or fire-cured tobacco that is powdered or ground for use as nasal or oral snuff, cut and grated for use as oral snuff, or stripped and compacted for use as chewing tobacco. These products routinely include formaldehyde, various sugars (most commonly sucrose, fructose, sorbitol, molasses, or dried fruit), water, sodium chloride, ammonium chloride, licorice, menthol, paraffin oil, and glycerol, in addition to tobacco-specific nitrosamines.[1] Tobacco also contains nicotine, which acts on both the parasympathetic and sympathetic nervous systems by binding to acetylcholine receptors. Nicotine is readily absorbed through the lungs, skin, GI tract, and mucous membranes. While ingestion is the most common route of exposure for accidental overdoses, exposure can also occur through the dermal, ocular, and inhalational routes. Compared to smoked tobacco, smokeless tobacco produces a much slower onset and much lower peak concentration of nicotine in the blood with the same total daily dose of nicotine.[2] However, studies comparing the use of smokeless versus smoked tobacco have demonstrated qualitatively similar magnitude of effects on the sympathetic nervous system from nicotine.[2]
Although nicotine toxicity is not a new phenomenon, the recent emergence of electronic cigarettes has spawned a market for highly concentrated liquid nicotine, resulting in unprecedented access to potentially toxic doses of nicotine and other harmful compounds in the home. Calls to Poison Centers regarding tobacco products have rapidly increased since 2010, resulting in an average of 200 calls per day in early 2014.[3]
A recent comprehensive review by Mayer suggests an LD50 of 6.5-13 mg/kg (approximately 500-1000 mg for adults), which is more consistent with reported values in case reports of actual fatalities.4 However, clinically significant symptoms of nicotine toxicity can occur in children with doses as low as 1 mg and in adults with doses as low as 2-5 mg.[4] For comparison, one cigarette has about 20-30 mg of nicotine, and the typical systemic dose from a single exposure to a cigarette, snuff or chewing tobacco is estimated to be 2 to 3 mg.[5]
What are the clinical features of nicotine toxicity?
Acute nicotine poisoning has a strongly biphasic pattern, owing to its short half life of one to four hours (Figure 2). The early clinical phase occurs most commonly within the first hour of exposure, and is characterized by excessive nicotinic stimulation. Patients may present with nausea, vomiting,
pallor, abdominal pain, salivation, bronchorrhea, tachypnea, hypertension, tachycardia, miosis, ataxia, tremor, fasciculations, arrhythmias (including atrial fibrillation), and seizures.[6] The delayed phase consists of central nervous system, as well as respiratory depression, and most commonly occurs greater than one hour after ingestion. These patients present with severe dyspnea, bradycardia, hypotension, shock, mydriasis, weakness, muscle paralysis, coma, and death. Signs and symptoms after ingestion of nicotine appear to be dose related, with lower doses stimulating the neural and cardiovascular systems, while higher doses suppress the central nervous and respiratory systems.
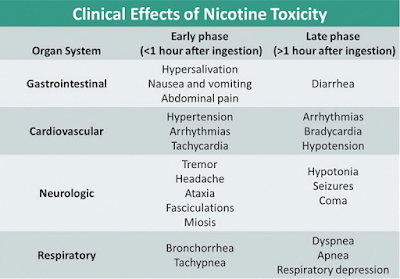 |
| Figure 2. The clinical features of nicotine toxicity by organ system, in the early (<1 hour after ingestion) and delayed (>1 hour after ingestion) phases. |
What treatments are available for nicotine toxicity?
Treatment of nicotine poisoning is usually supportive (Figure 3). The patient should have cardiorespiratory monitoring, intravenous access, and be observed closely. Immediate treatment should be initiated whenever nicotine toxicity is suspected, primarily focusing on resuscitating the patient and correcting any life-threatening symptoms, including respiratory support with mechanical ventilation if necessary. Anticholinergic drugs such as atropine can be given to counteract bradycardia, bronchorrhea, excessive salivation, and wheezing.6 Benzodiazepines may be given for seizures, and antiemetics may be given for nausea or vomiting. Decontamination by washing the skin and removing clothes is necessary for dermal exposures. Use of activated charcoal is an option for patients who present within an hour of ingestion, but it is infrequently used, and close consultation with your local Poison Control Center is recommended. Multi-dose activate charcoal may be beneficial to remove Figure 3. Treatments for nicotine toxicity by clinical manifestation. it from enterohepatic circulation. Likewise, gastric decontamination may be initiated if recommended by poison control experts. Although nicotinic stimulation, including hypertension and tachycardia, is usually treated with adrenergic antagonists during the early phase, this treatment is not recommended, as this may exacerbate any hypotension during the delayed phase.7 Hemodialysis may also theoretically enhance elimination due to its low protein binding and small volume of distribution but evidence supporting its use is sparse. While nicotine toxicity is commonly a clinical diagnosis, blood tests may be indicated, particularly if the patient is unstable, has an unclear history, ingestion was an attempted suicide, or if the toxidrome is inconsistent. Serum nicotine and cotinine (a nicotine metabolite) levels are not generally available and may not result in a timeframe that is practical in the ED. It may be useful to confirm exposure and toxicity.8 Generally, a minimum observation time after oral or dermal exposure is four to six hours, although longer observation periods may be warranted for large ingestions involving intact nicotine patches or plant material.
 |
| Figure 3. Treatments for nicotine toxicity by clinical manifestation. |
Conclusion
As tobacco delivery devices, particularly e-cigarettes, are becoming more widespread in the United States, more patients are presenting with sequelae of their toxicity. While most providers already know the classic presentation of nicotine toxicity, it is important for us to be aware of the other complications, including dysrhythmias, and their appropriate treatment.
References:
1. Hoffmann D, Adams JD, Lisk D, Fisenne I, Brunnemann KD. Toxic and carcinogenic agents in dry and moist snuff. J Natl Cancer Inst. 1987;79(6):1281-6.
2. Benowitz NL. Cardiovascular toxicity of nicotine: pharmacokinetic and pharmacodynamic considerations. In: Benowitz NL, ed. Nicotine Safety and Toxicity. New York, NY: Oxford University Press Inc; 1998:19–28.
3. Chatham-Stephens K, MD1, Law R, Taylor E, et al (2014). Notes from the Field: Calls to Poison Centers for Exposures to Electronic Cigarettes — United States, September 2010–February 2014 Weekly. 63(13); 292-293.
4. Mayer B. How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious self-experiments in the nineteenth century. Arch Toxicol. 2014;88(1):5-7.
5. Hukkanen J, Jacob P, Benowitz NL. Metabolism and disposition kinetics of nicotine. Pharmacol Rev. 2005;57(1):79-115.
6. Mishra A, Chaturvedi P, Datta S, Sinukumar S, Joshi P, Garg A. Harmful effects of nicotine. Indian J Med Paediatr Oncol. 2015;36(1):24-31.
7. Karaconji IB. Facts about nicotine toxicity. Arh Hig Rada Toksikol. 2005;56(4):363-71.
8. Raja M, Garg A, Yadav P, Jha K, Handa S. Diagnostic Methods for Detection of Cotinine Level in Tobacco Users: A Review. J Clin Diagn Res. 2016;10(3):ZE04-6.
