 |
| Image Source: Pixabay |
 |
| This post was peer reviewed. Click to learn more. |
Author: Ashley Grigsby, DO, PGY-4
Indiana University
RSA Social Media Committee Member
For many emergency physicians, the scariest patient to come through the doors is the crashing neonate. But make that same neonate a child with congenital heart disease (CHD) and you have a recipe for the so-called, “Code Brown.” One of the most unstable types of CHD is Hypoplastic Left Heart Syndrome (HLHS), a ductal dependent lesion that can be stabilized in the first few weeks of life with intravenous prostaglandins while awaiting surgical management. All patients with HLHS or single ventricle physiology, will require a stage 1 palliative surgery which is usually the Norwood procedure. Norwood patients are, arguably, the sickest of all CHD kids and are the most vulnerable to sudden death, leading many to live by the mantra, “Never trust a Norwood.”
Hypoplastic Left Heart Syndrome (HLHS) is a CHD characterized by underdevelopment of the left heart structures including the mitral valve, left ventricle, aortic valve and aorta. Review of Figure 1 illustrates the flow of blood in a patient with HLHS. You will notice that given the lack of left-sided outflow from the heart, a patent ductus arteriosus (PDA) is required to maintain mixing of oxygenated and de-oxygenated blood. This mixing is essential to maintain oxygen delivery to tissues; in the newborn period, prostaglandins, which keep the ductus arteriosus open, are started as soon as this diagnosis is made to maintain this mixing.
Prior to the 1980s, these children had a 100% mortality rate in the first few weeks to months of life.[1] However, since this time, surgical advances have been made in which these children undergo a series of three surgeries that have increased survival to early adulthood and beyond. Stage 1 of the series is usually the Norwood procedure.[1] In the first few weeks of life, these children’s hearts are too small for full correction, thus the staging of procedures to allow the child to grow before final surgical correction. The Norwood stage ranks highest in operation mortality among congenital heart surgeries, and the period between stage 1 and stage 2 has a mortality rate of 15-30%, depending on the care center.[1,2] After patients undergo the Norwood procedure, they are discharged home with close home monitoring with their pediatric cardiologist until four to six months of age when they an undergo stage 2 surgery.
The Norwood procedure consists of three major steps: (1) creation of neoaorta using the main pulmonary artery (PA) and the aortic arch, (2) placement of a modified Blalock-Taussig (BT) shunt from the innominate artery to the right pulmonary artery, and (3) resection of the atrial septum.[2] The resulting heart is pictured in Figure 2. Deoxygenated blood returns to the right atrium and is pumped through the neoaorta via the right ventricle. The BT shunt now provides all the pulmonary blood flow. Oxygenated blood from the lungs returns to the left atrium and crosses a hole in the atrial septum to mix with deoxygenated blood from the body. This mixing of oxygenated and deoxygenated blood is the reason that oxygen saturations remain low. The normal oxygen saturation for a Norwood is 75-85%. This is very important to remember when it comes to troubleshooting in sick Norwood patients.
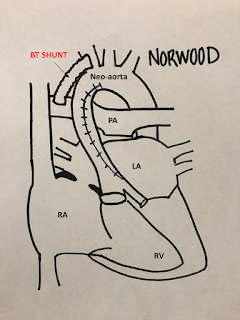 |
| FIGURE 2: Heart following the Norwood operation |
If a Norwood patient’s oxygen saturation is 75-85% and they are placed on supplemental oxygen, the excess oxygen will cause dilation of pulmonary vasculature. This changes pressure gradients and causes increased shunting towards the pulmonary system, which leads to pulmonary edema and can lead to sudden death. Remember to always ask parents what the child’s normal saturation is before placing on oxygen.
When approaching these patients, if you can remember the anatomy and flow, pictured in Figure 2, you can determine the best way to treat. It is sometimes easiest to separate these patients into two groups: saturations too high (>85%) or saturations too low (<75%). In patients with saturations >85%—the most common issue is re-coarctation of the aorta. Increase in afterload from a re-coarctation of the aorta leads to increase in shunting to the pulmonary bed and more oxygenated blood than de-oxygenated blood.[2]
The cause of low oxygen saturations (<75%) is more difficult to determine. These patients are very sensitive to fluid shifts and anything that decreases preload—viral syndromes, decreased PO intake/dehydration—can decrease blood supply to the pulmonary system, resulting in less oxygenation. Low saturations can also occur when there is a problem with the BT shunt. Remember, these children are completely dependent on this shunt for blood flow to the lungs, and thus oxygenation. If the shunt clots off, patients will quickly suffer hypoxic cardiac arrest; however, if a partial thrombosis or stenosis develops, they can present with low oxygen saturations (less than 75%). If a Norwood patient has oxygen saturation less than 75%, it is okay to apply supplemental oxygen, making the goal 75-85%, but not allowing them to be greater than 85%.[2] Other causes of low saturations include issues with the atrioventricular valves and worsening ejection fraction of the right ventricle.
Although Norwood patients are a small subset of CHD, many similar principles apply to other forms of cyanotic CHD. Patients with CHD are very sensitive to fluid shifts and balances as well as oxygen supplementation. It is important to always assess fluid status carefully, and when needed, replace with intravenous fluids in small increments, 5-10 ml/kg at a time. It is also very important to ask parents the patient’s normal oxygen saturation baseline and only supplement oxygen to that saturation. Don’t be afraid to call a friend! The patient’s pediatric cardiologist will likely be eager to help you manage these patients and get them to definitive care quickly.
References:
1. Yabrodi M, Mastropietro CW. Hypoplastic left heart syndrome: from comfort care to long-term survival. Pediatr Res. 2017;81(1-2):142-149.
2. Marshall A. Hypoplastic Left Heart Syndrome. Up to date. 2017. Accessed on 28 September 2017. Available from: https://www.uptodate.com/contents/hypoplastic-left-heart-syndrome?source=search_result&search=hypoplastic%20left%20heart%20syndrome%20children&selectedTitle=1~44

