 |
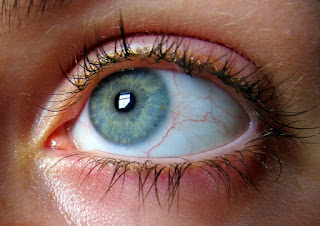
| Image Credit: Flickr |
 |
| This post was peer reviewed. Click to learn more. |
Author: Fernando Pellerano, MS-V
Universidad Iberoamericana (UNIBE) School of Medicine
Overview
Retinal artery occlusion (RAO) is considered a true ophthalmic emergency requiring immediate assessment and initiation of treatment. Appropriate initial emergency management may be the most important factor in determining visual outcome.[1]
RAO can either be central or branch. Central retinal artery occlusion (CRAO) results from a blockage anywhere between the origin of the artery (off the ophthalmic artery), to its first branch at the entry to the retina.[2] The site of obstruction is therefore not generally visible on ophthalmoscopy and in most cases the entire retina is affected. Branch retinal artery occlusion (BRAO) occurs when the blockage is distal to the optic nerve, within the visible vasculature of the retina. A BRAO can involve as large an area as three quarters of the retina, or as small an area as just a few micrometers.[1]
Epidemiology and Etiology
Incidence of RAO is approximately one per 100,000 per year and increases with age, peaking in the sixth and seventh decades. The central retinal artery is more commonly blocked than the branch retinal artery. [1] Although many systemic diseases are associated with RAO, more than 50 % of all affected patients will manifest no apparent systemic or local causes for the retinal disease.[2] Possible Etiology and Risk Factors for both CRAO and BRAO are listed in Table 1 and Table 2.[3, 4]
|
Table 1. Etiology of CRAO and BRAO.
Image A. Cholesterol Emboli (Hollenhorst Plaque). Image B. Calcium Plaque. Image C. Platelet- Fibrin Clot. |
Presentation and Differential Diagnosis
Patients with CRAO describe painless, unilateral, acute loss of vision (count fingers to light perception in 94% of eyes) or abrupt loss of partial visual field in BRAO occurring over seconds and may report a history of Amaurosis Fugax (transient, painless unilateral vision loss) before presentation. The pupil may be dilated with sluggish reaction to light or present with a marked RAPD (Relative Afferent Pupillary Defect). If vision loss is acute, transient and bilateral other causes such as migraine auras, heart failure and hypertensive emergencies should be suspected.[3, 4] Pain is not generally a part of RAO unless some underlying disease is present (ex: Giant Cell Arteritis, Ocular Ischemia).[1]
In some patients, an artery derived from the choroidal circulation, called the cilioretinal artery, may perfuse a small amount of the central retina. This artery, which is present in up to 20% of individuals, remains patent in CRAO. Some of the visual field corresponding to the territory of the patent cilioretinal vessel can be spared in selected individuals. This will lead, rarely, to a patient with normal central vision, but constricted peripheral visual fields.[1]
Funduscopy examination after CRAO reveals interrupted columns of blood within the retinal vessels (sometimes referred to as “Boxcarring”) and retinal pallor secondary to retinal edema, with a characteristic cherry red spot at the fovea (See Image D) and attenuation of the retinal artery.[4] A cherry red spot occurs in CRAO because of the retinal whitening of the surrounding nerve fiber layer. The fovea itself has no nerve fibers, so its appearance does not change significantly from normal. The retinal whitening surrounding the normal reddish tint of the macular area produces the cherry red spot.[1] Splinter retinal hemorrhages on the disc are common. Important differential diagnoses are listed in Table 3.[3]
|
Table 2. Risk Factors Associated to CRAO and BRAO.
Table 3. Important Differential Diagnosis of RAO. Image D. Central Retinal Artery Occlusion disclosing Cherry Red Spot at the fovea. |
Work up and Treatment
For immediate initial management, emergency physicians should follow these basic steps and tips:
1) Anecdotal evidence of success in restoring circulation suggest that the following treatments should be instituted within 90 to 120 minutes of the occlusive event:[3]
- a. Hyperventilation into a paper bag to induce a respiratory alkalosis and subsequent vasodilation.[3]
- b. Intraocular pressure reduction with acetazolamide, 500 mg IV, or two 250 mg tablets p.o. or a topical beta-blocker (e.g., Timolol or Levobunolol 0.5% b.i.d).[4,5]
- c. Immediate ocular massage in order to plunge an embolus farther along the vasculature into a distal branch, minimizing the area of ischemia and vision loss.[4,5]
- d. Increase oxygenation to the retina by having the patient inhale a mixture of 95% oxygen and 5% carbon dioxide (carbogen) for 10 minutes every 2 hours for 24- 48 hours after the blockage. It should not be used in a patient with chronic obstructive pulmonary disease; use hyperbaric oxygen therapy instead.[1]
- e. Administering oral nitrates and laying the patient flat on his or her back.[2]
2) Thrombolytics have not shown any benefit in recent trails.[2]
3) Immediate ESR, CRP and platelets to rule out giant cell arteritis (GCA) if the patient is 55 years of age or older. If the patient’s history, laboratories or both are consistent with GCA, start high dose systemic steroids.[3]
4) Check blood pressure.[3]
5) Perform blood test depending on clinical history: Fasting blood sugar, glycosylated hemoglobin, complete blood count (CBC) with differential, prothrombin time and activated partial thromboplastin time (PT/PTT).[3]
6) In patients younger than 50 years or with appropriate risk factors or positive review of systems, consider lipid profile, antinuclear antibody (ANA), rheumatoid factor, Fluorescent treponemal antibody (FTA/ABS), serum protein electrophoresis and hemoglobin electrophoresis.[3]
7) After acute management of RAO, perform a carotid artery evaluation by duplex dopler ultrasonography.[4]
8) Cardiac evaluation with electrocardiography (ECG), echocardiography and possibly holter monitoring should be contemplated.[3]
9) Consider consultation with an ophthalmologist immediately when RAO is suspected because irreversible damage occurs in as little as 100 minutes of occlusion.[4,6] Because the inner retina is highly sensitive to loss of perfusion, intervention is rarely, if ever, attempted in anyone with an obstruction more than 72 hours old.[1]
10) Consider referral to an internist for a complete work up and minimization of risk factors with diet and lifestyle modifications and treatment of underlying conditions.[4,7]
Overall, when talking about retinal artery occlusion, all efforts should be geared towards restoration of circulation before referral to an ophthalmologist in order to improve visual prognosis.
References
1. Gault J, Vander. Retinal Arterial Obstruction In Ophthalmology Secrets. 4th edition. Philadelphia, PA: Elsevier, Inc.; 2016.
2. Borooah S, Wright M, Dhillon . Retinal Artery Occlusion and Amaurosis Fugax In Ophthalmology Pocket Tutor.1st ed. London, UK: JP Medical Ltd; 2013.
3. Gerstenblith A, Rabinowitz M. Central Retinal Artery Occlusion & Branch Retinal Artery Occlusion In Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.
4. Pokhrel P, Loftus S. Ocular Emergencies. Am Fam Physician. 2007; 76(6) 829-836. PMID: 17910297
5. Duxbury O, Bhogal P, Cloud G, Madigan J. Successful treatment of central retinal artery thromboembolism with ocular massage and intravenous acetazolamide. BMJ Case Rep. 2014; 2014 PMID: 25480141.
6. Varma D, Lee AW, Chen CS. Reply: ‘a review of central retinal artery occlusion: clinical presentation and management’. Eye (Lond). 2014;28(10):1270.
7. Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond). 2013;27(6):688-97.
Images and Tables:
1. Table 1 is adapted from Gerstenblith A, Rabinowitz M. Central Retinal Artery Occlusion & Branch Retinal Artery Occlusion In Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.
2. Image A, B and C are freely available in http://www.studydroid.com/index.php?page=viewPack&packId=59507 under the topic ocular Disease 2 – Midterm Vascular created by erikiksaz and is used according to terms described in Creative Commons Attribution 2.5 license.
Table 2 is adapted from Pokhrel P, Loftus S. Ocular Emergencies. Am Fam Physician. 2007; 76(6) 829-836. PMID: 17910297.
Table 3 is adapted from Gerstenblith A, Rabinowitz M. Central Retinal Artery Occlusion & Branch Retinal Artery Occlusion In Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.
Image D is freely available in http://www.kellogg.umich.edu/theeyeshaveit/non-trauma/artery-occlusion.html under the topic Central Retinal Artery Occlusion created by Jonathan Trobe, M.D, University of Michigan Kellogg Eye and © The Reagents of the University of Michigan and is used according to terms described in Creative Commons Attribution 3.0 license.
