Author: Peter Malamet OMS- IV
Philadelphia College of Osteopathic Medicine
 |
| This post was peer reviewed. Click to learn more. |
Recently, I heard a quote that has summarized a large part of the emergency medicine practice I have experienced thus far. My attending said, “In a few years, ultrasound will be the new stethoscope.” What he was referring to is not only how popular ultrasound is becoming, but the necessity for physicians to be able to use ultrasound correctly. Ultrasound can help keep certain patients right where we want them, not in a CT scanner, but in our emergency room where we can adequately diagnose and treat them. Ask any physician in the hospital, the last place they want an unstable (or potentially unstable) patient is in the radiology suite. From the Focused Assessment with Sonography in Trauma (FAST) exam to a simple post void residual, ultrasound is a fantastic tool. In this article I will present a relatively newer type of ultrasound technique as an example showing how important this tool can be.
The optic nerve sheath ultrasound was recently introduced to me, and needless to say it is an amazing diagnostic tool. This is an excellent way to possibly avoid an unnecessary CT scan. There are numerous publications describing the use of optic nerve sheath ultrasound for the evaluation of intracranial pressure (ICP). Studies have shown a high sensitivity and negative predicative value in its use to detect and increase of ICP.[1,2] Qayyum and Ramlakhan found a sensitivity and specificity of 100% and 75% respectively, along with a positive and negative predictive value of 95.4% and 100% respectively.[1] Tayal and colleagues also noted a sensitivity of 100%, with a slightly lower specificity of 63%.[2] This technology has been around for many years and seems as though it will only increase in popularity; therefore, it would behoove emergency medicine students, residents and attendings to have some knowledge of the procedure.
Studies have shown that the first sign of increased intracranial pressure is seen in dilation of the optic disk.[1] As intracranial pressure increases, the CSF can push against the nerve enough to dilate its sheath.[1] The ultrasound will measure the width of this optic nerve sheath, with greater than 5mm (some sources say 6mm) signifying an abnormal result.[2,3] The ultrasound is performed in a supine patient, using a 7.5MHz linear probe over their eyelid. The optic nerve sheath will be the black stripe running down the posterior aspect of the globe.[2] It should be running down the center of the monitor if you have correct placement. You simply measure 3mm down the posterior aspect of the eye, then across that area of the sheath.[2] Measurements should be taken in both eyes, due to the possibility of unilateral papilledema.[1] Once again, a measurement over 5mm correlates with elevated intracranial pressure. An excellent website to visit for a detailed explanation and photos is http://www.sonoguide.com/smparts_ocular.html.[4]
Imagine a patient with a hypertensive emergency, head trauma, or encephalopathy. The patient will most likely require a CT scan at some point; however, a physician can consider initiating treatment to lower ICP after a positive ultrasound exam. In a syndrome, such as an intracranial bleed, where minutes can drastically change the clinical course, ultrasound provides an even better diagnostic evaluation.
Ultrasound’s importance in the diagnosis of numerous pathologies continues to increase. A high level of clinical exposure is critical to becoming skillful in the use of ultrasound. The key is to not only be able to perform the ultrasound but also accurately interpret the results without the help of a radiologist. This tool leads to a quicker diagnosis and thus faster treatment and disposition of patients; however, it will only go as far as the individual performing the study.
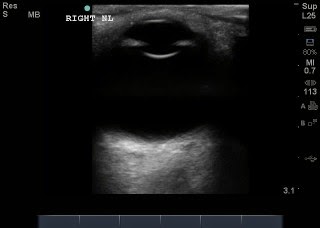
This is an ultrasound image of the normal eye showing the small black stripe posterior to the globe (bottom of image), which is the optic nerve.
Optic Nerve Sheath Diameter (ONSD) measured: Example of measuring the optic nerve sheath. A is the initial measurement going down the length of the nerve, 3mm. B is the width of the nerve sheath, 4.1mm (normal).
References:
1. Qayyum H, Ramlakhan S. Can ocular ultrasound predict intracranial hypertension? A pilot diagnostic accuracy evaluation in a UK emergency department. European Journal Of Emergency Medicine [serial online]. April 1, 2013;20(2):91-97.
2. Tayal V, Neulander M, Norton H, Foster T, Saunders T, Blaivas M. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Annals Of Emergency Medicine [serial online]. April 2007;49(4):508-514.
3. Smith E, Amin-Hanjani S. Evaluation and Management of Elevated Intracranial Pressure in Adults. UpToDate. http://www.Uptodate.com. Accessed July 15, 2014.
4. Adhilari SR, Small Parts- Ocular Ultrasound. Ultrasound Guide for Emergency Physicians. http://www.sonoguide.com/smparts_ocular.html. Accessed August 19, 2014.